In the normal course of pregnancy, prenatal contractions of the uterus are noted closer to its end, which are most often painless, mostly occur at night and lead to shortening and softening of the cervix, and opening the cervical canal.
The main types of anomalies of labor include pathological preliminary period, primary and secondary weakness of labor, excessively strong labor, discoordination of labor and tetanus of the uterus.
Pathological preliminary period
In contrast to normal prenatal uterine abnormalities, the pathological preliminary period is characterized by spastic, painful and erratic contractions of the uterus and the absence of structural changes from the cervix, which is a sign of prenatal dysfunction of its contractile function. Pathological preliminary period can last up to several days. A frequent complication of the pathological preliminary period is untimely rupture of amniotic fluid. The main reasons that lead to the development of this complication are: nervous stress; endocrine and metabolic disorders; inflammatory changes in the uterus, the age of primiparous older than 30 years and younger than 17 years.
Treatment of the pathological preliminary period should be aimed at accelerating the "maturation" of the cervix, the removal of uncoordinated painful contractions of the uterus. With fatigue and irritability, the patient is prescribed medication sleep, rest, sedatives (motherwort tincture, collection of sedative herbs, valerian root); antispasmodics; painkillers; β-mimetics (ginipral, partusisten). For urgent preparation of the cervix for childbirth using drugs based on prostaglandin E2, which are injected into the cervical canal or posterior vaginal fornix. The duration of the treatment of the pathological preliminary period should not exceed 3-5 days. With a "mature" cervix, taking into account the favorable obstetric situation, it is possible to open the femoral bladder early and to give birth through the birth canal. In the absence of the effect of therapy, maintaining the "immaturity" of the cervix, it is advisable to cesarean section.
Weak labor activity
The weakness of labor is characterized by insufficient strength and duration of uterine contractions, an increase in the intervals between contractions, a violation of their rhythm, a slowing down of the opening of the cervix, a delay in the progress of the fetus. Distinguish between primary and secondary weakness of labor. With primary weakness, contractions from the very beginning of labor are weak and ineffective. Secondary weakness occurs against the background of the normally begun labor activity. The weakness of labor leads to a prolonged course of labor, fetal hypoxia, fatigue of the woman in labor, lengthening of the anhydrous period, infection of the birth canal, development of inflammatory complications, bleeding during childbirth and the postpartum period. The causes of generic weakness are very numerous. The main ones are violations of the mechanisms regulating the generic process, which include: changes in function nervous system as a result of stress, endocrine function disorders, menstrual disorders, metabolic diseases. In a number of cases, the weakness of the labor forces is due to such pathological changes in the uterus as malformations, inflammation, and overdistension. Lack of contractile activity during childbirth is also possible with a large fetus, with multiple fetuses, polyhydramnios, uterine myoma, post-term pregnancy, in women with severe obesity. Among the causes of secondary weakness of labor activity, besides those already mentioned, fatigue of the parturient woman as a result of prolonged and painful contractions, obstruction of the newborn fetus due to incompatibility of the head and pelvis, with the wrong position of the fetus, with the presence of a tumor in the small pelvis should be noted.
The main method of treatment of the weakness of labor activity is spontaneous stimulation with an opened fetal bladder, which consists in intravenous drip infusion. drugsthat enhance the contractile activity of the uterus (oxytocin, prostaglandin F2a). A significant effect in treating weakness of the labor forces can be obtained by combining prostaglandin F2a with oxytocin. With fatigue of the woman in labor, detection of weakness of labor forces at night, with a poor readiness of the cervix for childbirth or a small opening of it, treatment should begin with giving the woman a rest for 2 to 3 hours (obstetric anesthesia). Otherwise, the conduct of birth stimulation may further complicate the course of labor. After a rest, a vaginal examination is performed to determine the obstetric situation and the condition of the fetus is assessed. After sleep, labor activity may increase, and further treatment is not required. If the labor activity is still insufficient, uterine-stimulating agents are prescribed. Contraindications to the stimulation of labor are: the discrepancy between the size of the fetus and the pelvis of the mother, the presence of a scar on the uterus after cesarean section or after the removal of uterine fibroids, symptoms of a threatening uterine rupture, preceding severe septic diseases of the genital organs. If the introduction of drugs that enhance uterine contraction within 2 hours does not show the dynamics of cervical dilatation or the condition of the fetus is worsening, then further administration of drugs is not appropriate. In this situation, the question should be addressed in favor of operative delivery. The choice of method depends on the specific obstetric situation. With the weakness of labor in the first stage of labor, cesarean section should be performed. In the second stage of labor, it is advisable to overlay the output obstetric forceps or perform vacuum extraction.
Stormy labor activity
Excessively strong, stormy labor activity is characterized by very strong and / or frequent contractions and attempts (after 1–2 minutes), which can lead to swift (1-3 h) or fast (up to 5 h) births. Expulsion of the fetus occurs sometimes for 1-2 attempts. Stormy generic activity is dangerous to the mother and fetus. In the parturient women often have deep ruptures of the cervix, vagina, clitoris, perineum; possible premature detachment normally located or the development of bleeding. Frequent, very strong contractions and rapid expulsion of the fetus often lead to hypoxia and birth trauma to the fetus.
When correcting for vigorous labor, the woman is given a position on the side opposite to the position of the fetus, which she retains until the end of the birth. Get up pregnant woman is not allowed. For the regulation and removal of excessive labor, intravenous administration of magnesia sulphate, tocolytic drugs (partusisten, gynipral, etc.) is used, seeking to reduce the number of contractions to 3-5 in 10 minutes.
Tetanus uterus
Uterus tetany is rare. In this case, the uterus does not relax at all, and all the time remains in a state of tonic tension, which is caused by the simultaneous occurrence of several pacemakers in different parts of the uterus. At the same time, contractions of various uterine regions do not coincide with each other. There is no cumulative effect of the contraction of the uterus, which leads to a slowing and stopping of labor. Due to a significant violation of the uteroplacental circulation, severe fetal hypoxia develops, which is manifested in a violation of its cardiac activity. The degree of disclosure of uterine throat is reduced compared with the previous vaginal examination. The woman can increase body temperature and develop chorioamnionitis, worsening the prognosis for the mother and fetus. Uterus tetany can be one of the symptoms of such serious complications as threatening or beginning uterine rupture, premature detachment of the normally located. The reasons for this anomaly are the presence of significant obstacles to the progress of the fetus, a narrow pelvis, a tumor, an unreasonable, erroneous prescription of family-stimulating drugs.
In the treatment of tetany of the uterus using anesthesia. Often, after anesthesia, labor activity normalizes, and childbirth ends spontaneously. With tetany of the uterus, which is a symptom of its rupture, with premature detachment of a normally located placenta, a cesarean section is performed to mechanically prevent the passage of the fetus. If there is a complete opening of the cervix, then the fetus is extracted under anesthesia using obstetric forceps or by the leg (with pelvic presentation).
Discordination of labor
Discoordination of labor activity is characterized by indiscriminate contractions of various parts of the uterus due to the displacement of the pacemaker zone. At the same time there may be several such zones. At the same time, the synchronicity of contraction and relaxation of certain parts of the uterus is not observed. The left and the right halves of the uterus may be out of sync, but more often it refers to the disruption of the contraction processes in its lower part. The contractions become painful, spastic, uneven, very frequent (6-7 in 10 minutes) and long. Between contractions, the uterus does not completely relax. The behavior of the woman in labor is restless. There may be nausea and vomiting. Observed difficulty urinating. Despite frequent, strong and painful contractions, disclosure of uterine throat occurs very slowly or does not progress at all. At the same time, the fetus is hardly moving along the birth canal. Due to violations of the uterus contraction, as well as due to incomplete relaxation of the uterus, severe fetal hypoxia often develops between contractions, and intracranial trauma of the fetus is also possible. Discordination of uterine contractions often causes untimely rupture of the amniotic fluid. The cervix becomes dense, the edges of the uterine throat remain thick, taut and can not be stretched. The development of discoordinated labor activity is promoted by the negative attitude of the woman in childbirth to childbirth, the age of the first birth mother older than 30 years, the untimely rupture of the amniotic fluid, rough manipulations in the process of childbirth, developmental anomalies and tumors of the uterus.
In the treatment of discoordination of labor, which is aimed at eliminating excessive uterine tone, use sedatives, drugs eliminating spasm, painkillers and tocolytic drugs. The most optimal method of pain relief is epidural anesthesia. Deliveries are carried out with constant medical monitoring and monitoring of the fetal heart and uterine contractions. With ineffective treatment, as well as in the presence of additional complications, it is advisable to perform a cesarean section without an attempt to carry out corrective therapy.
Prevention of labor abnormalities
In order to prevent anomalies of labor, careful adherence to the treatment and protection regime, careful and painless management of labor is necessary. Drug prophylaxis is carried out in the presence of risk factors for the development of anomalies of uterine contractile activity: young and elderly age primiparous; burdened obstetric and gynecological history; indication of chronic infection; the presence of somatic, neuroendocrine and neuropsychiatric diseases, vegetative-vascular disorders, structural inferiority of the uterus; ; overstretching of the uterus due to polyhydramnios, multiple fetuses or large fetuses.
Women at risk of developing abnormal labor should be given physiopsycological and prophylactic training for childbirth, trained in muscle relaxation, muscle tone control, and skills for reducing anxiety. Night sleep should be 8-10 hours, day rest not less than 2-3 hours. Provides for a long stay in the fresh air, a balanced diet.Childbirth is a physiological (that is, natural, natural) process during which expulsion from the uterus through the birth canal of the fetus and placenta occurs. The causes of the onset of labor are very complex and diverse: by the end of the pregnancy, numerous changes occur in the future mother's body:
- significantly increased excitability of the nervous elements and muscles of the uterus;
- the uterus begins to actively respond to various stimuli;
- the growth of the baby during this period is ahead of the accumulation process, parts of its body more closely contact with the wall of the uterus.
- the head of the fetus (and, in the case of pelvic presentation, the buttocks), descends below and irritates especially excitable nerve plexuses located in the lower segment of the uterus.
- at the same time, the production of hormones and hormone-like substances increases in the body of the future mother, which, acting on the nerve endings in the uterus muscle, increase its tone and ability to contract;
- in the last two weeks before birth, the production of estrogens increases, causing uterus to arouse, and the amount of progesterone, the pregnancy hormone, gradually decreases. When the excitability of the uterus and the strength of the stimuli reach a certain limit, there is a regular labor activity.
Childbirth is a complex process that occurs reflexively and is regulated by the nervous and hormonal systems. Each contraction of the uterus - contraction - is accompanied by irritation of the nervous elements in its wall. In this case, the nerve endings secrete biologically active substances that contribute to the occurrence of the next uterine contraction. Thus, the entire process is controlled from the beginning to the very end of the genera through a closed chain.
Why birth does not begin?
So, normally, the birth is started by the body of the future mother independently - at the moment when both the main participants, mother and baby, are fully prepared for this important event. However, as in other natural processes, various failures sometimes occur during pregnancy and at the stage of preparation for childbirth, and then childbirth does not begin on its own, despite the baby’s full readiness for birth. Such a condition in obstetrics is referred to as a tendency to and requires medical intervention.
What can cause a delayed start, why labor does not begin in a timely manner and how to notice it in time? Consider the most common causes.
Biological immaturity of the birth canal
This term refers to the discrepancy between the state of the cervix and the walls of the vagina during pregnancy. Normally, before delivery, the cervix gradually shortens and begins to open slightly, the tissues of the vagina and cervix become soft and elastic. Changes in the birth canal usually occur at 37–39 weeks gestation. If during full-term pregnancy and a mature fetus (this data is confirmed by ultrasound) the cervix remains dense and long, as in mid-pregnancy, and the cervical canal is closed, it is necessary to prescribe a drug preparation of the birth canal. Otherwise, childbirth will not start on time: the same hormones that cause the onset of labor activity are responsible for the readiness of the cervix for labor, therefore the biological immaturity of the birth canal indicates a lack of estrogen in the body. We can say that the biological immaturity of the birth canal is for the physician an external manifestation of the problem, a kind of signal: the mother's body needs help in preparing for childbirth.
Polywater
This is not a rare complication of pregnancy and childbirth. The diagnosis of "polyhydramnios" can be made in the case when the amount of amniotic fluid reaches or exceeds 2 liters. The origin of this pathology of pregnancy is still not fully understood. The immediate cause of the increase in the number of fetal waters is always, in the end, the increased secretory activity of the cells of the membran of the membranes. The most common known cause of damage to the secretory epithelium of the fetal bladder is an infectious process involving the amnion. Most often, the membranes undergo a viral infection (viruses are very small and are able to enter the bloodstream through the placenta). Due to excess water, the baby does not descend and does not exert proper pressure on its head or buttocks on the cervix; This leads to biological immaturity of the birth canal (unavailability of the cervix and vaginal tissues for childbirth). With significant polyvody, childbirth can not only not start in time, but also proceed with serious complications. It is characteristic of the development of the so-called pathological prelaminar period, when the expectant mother during the day and more are worried about the incessant painful training bouts, however, the clan activity does not begin on its own.
Lack of water
This is a situation in which the amount of water falls short of the lower limit of normal (800 ml). The reasons for the insufficient number are different. Almost always, the main cause of oligohydramnios are various pathologies of the fetal membranes (amnion, or fetal bladder): it is the amnion that is responsible for the production and exchange of fetal fluid. Almost always, as a result of infection, the amnion suffers one of its most important functions - the exchange and production of fetal waters. The main symptom of true peeling is a gradual decrease in the functional activity of the fetal membranes and the placenta, which in turn affects the deterioration of the overall condition of the fetus. The scarcity of water during retreatment is associated with the aging of the amniotic membranes and the placenta. The lack of water and the increased density of the wall of the fetal bladder, as it were, inhibit the development of contractions from the inside. As a result, the baby begins to suffer from a lack of oxygen and pressure of the walls of the uterus, childbirth begins much later than the period and runs much longer and harder.
Premature aging of the placenta
Premature aging of the placenta is also called fetoplacental insufficiency, it is the loss of its main function as the placenta - the life support of the baby in the mother’s womb - for up to 40 weeks, when there is no question of repositioning. The cause of this pathology can be intrauterine infection, preeclampsia (late toxicosis of pregnancy, manifested in a violation of the work of the future mother’s kidneys) or an abnormality of the placenta structure. The diagnosis in this case is made according to ultrasound, doplerometry (study of blood flow in the vessels of the placenta, umbilical cord and uterine arteries) and cardiotocography. Such a diagnosis is a cause for medical labor induction regardless of the term of delivery - the deterioration of the placenta function leads to oxygen starvation baby and endangers his life.
Premature discharge of water
Premature outpouring of water in obstetrics means spontaneous rupture of the membranes and discharge of water in the absence of labor activity (contractions). The reason for such a scenario of the onset of labor can be high water, incorrect position of the fetus, thinning of the fetal bladder due to perenosheniya or infection, as well as an injury to the abdomen of the expectant mother (blow, fall). Most often, the outpouring of water is a signal to the body to the beginning of labor. However, if this does not occur within 6–8 hours, medical labor induction is necessary - a long anhydrous period threatens the mother and baby with serious infectious complications. An anhydrous interval is the time interval from the moment of rupture of the membranes to the birth of a baby. This interval is of great importance for predicting the development of complications. The fact is that in violation of the integrity of the fetal bladder, the last barrier between the sterile uterus and the non-sterile genital tract (vagina) disappears. The pathogens in the vagina ascend by penetrating the uterine cavity through a rupture in the membranes, affecting first the membranes and the placenta, then the mucous membrane of the uterus, and finally the fetus. For an anhydrous period of more than 12 hours, the uterus and fetus are considered infected. For the future mother, infection of the uterus threatens with the development of sepsis (blood infection), and for the baby, intrauterine infection is fraught with death due to impaired placental blood flow and infectious damage to the body.
On your marks
Obviously, with such serious deviations from the course, physicians have every reason to interfere in the natural development of the process and apply the necessary measures to remove obstacles to the timely start and safe delivery of labor. However, since the reasons for the “start delay” can be so different, then the measures for labor induction in each case will need their own.
With the biological immaturity of the birth canal, the expectant mother is prescribed antispasmodics - medicines that remove muscle tone from the cervix and help her to relax. Drugs can be administered intravenously, intramuscularly or topically, in the form of rectal or vaginal suppositories.
If the immaturity of the birth canal is combined with re-stabbing, a Foley catheter can be used — a flexible, elastic, thin tube with an inflating balloon at the end. A catheter is inserted into the cervical canal and the balloon is inflated with the aid of injected fluid. The bulb inflated inside the cervix exerts mechanical pressure on its walls and promotes opening.

If the catheter does not start delivery, after its extraction, prostaglandins are injected into the cervical canal, which contain substances that provide hyperelasticity, stretchability and decrease pain sensitivity of the cervix, vaginal walls and perineal skin, and also help the future mother's body to quickly accumulate The required amount of hormones to start. Such a powerful medical preparation of the tissues of the birth canal is never carried out without indications and is prescribed only in a hospital.
In case of detected polyhydramnios, shallow water, as well as during post-aging and premature aging of the placenta, a planned amniotomy is prescribed. This term in obstetrics means puncture of the fetal bladder in order to provoke the onset of labor. The amniotomy procedure itself is absolutely painless and safe for mother and baby - there are no nerve endings in the fetal bladder, so its puncture is in principle not sensitive for the future mother. It is also impossible to damage the fetal head or the walls of the birth canal - the instrument with which amniotomy is carried out, atraumatic - it is smooth and has no protruding sharp parts. The fetal bladder is opened using an amniotomy, a sterile instrument resembling a crochet hook made of aseptic medical plastic. Near its end there is a small burr, with which the doctor picks up the fetal bladder under the control of the fingers in the course of a normal vaginal examination - this is enough to form a hole in the shell and pour out water. This manipulation is possible only when the birth canal is ready - in order to conduct an amniotomy, the doctor must be able to freely insert two fingers into the cervical canal. Therefore, if the problem that prompted amniotomy is combined with the biological immaturity of the birth canal, you must first apply the measures of drug preparation of the cervix - antispasmodics or the introduction of a Foley catheter.
In case of premature discharge of water in the absence of signs of labor activity (contractions), labor induction is used for 6–8 hours, that is, it causes the onset of contractions. For this purpose, a drug is used in obstetrics - a synthetic analogue of the natural hormone estrogen, which normally should be released in the body of the future mother and start the process of childbirth. It works only as a starting factor, without affecting the strength and speed of development of contractions. The drug is administered intravenously, very slowly (2–2.5 hours) - to maximize the re-establishment of the natural onset of labor.
What is perenashivanie?
Special measures to induce labor (induction of onset of labor) are taken only in case of fetus over-wearing. Moreover, repurposing is not just a pregnancy lasting for more than 40 weeks, as many mistakenly believe. Recall that pregnancy is considered full-term (and the child is ready for birth) from 38 to 42 weeks. 40 weeks is the most likely, but not exact, date of delivery. The term "perenash" denotes the failure of the auxiliary organs of pregnancy - the placenta and fetal membranes, their aging and deterioration of functions. These organs responsible for the life support of the fetus have their “shelf life”, after which they gradually lose their ability to protect the baby and maintain his life in the mother's body. Aging of the placenta and membranes gradually leads to oxygen starvation of the fetus, reduction of nutrition and metabolism. The prenatal environment of the baby also undergoes changes - the amount of water decreases, they become viscous; fetal membranes become denser and lose their elasticity, as a result, the walls of the uterus begin to put pressure on the fetus. These changes worsen the prognosis for childbirth and pose a risk to the health of the baby. Ultrasonography, Doppler (control of placental blood flow), CTG (fetal heartbeat monitoring) and amnioscopy (transvaginal optical examination of the fetal bladder and water) are used for accurate diagnosis. If the pregnancy lasts more than 40 weeks, but there are no signs of delay, the doctors only monitor the condition of the mother and baby, without undertaking any additional interventions.
One of the reasons leading to an increase in the incidence of newborns is still anomaly of labor activity. Among them, the most common weakness of labor activity. This pathology is distinguished by weak, short contractions that slow down not only the smoothing and disclosure of the cervix, but also the progress of the fetus through the birth canal of the mother. The weakness of the tribal forces is more common in primipara women.
Causes of poor labor
Various factors can cause weakness in labor:
- endocrine and metabolic disorders in the pregnant woman's body (obesity, thyroid gland insufficiency, diabetes mellitus);
- overstretching of the uterus (in the presence of multiple fetuses, large fetus, polyhydramnios);
- pathological changes in the wall of the uterus, developed as a result of previously transferred inflammatory process in the uterus, the presence of defective scar on the uterus after previous cesarean section or surgery for uterine fibroids;
- malformations of the uterus or its congenital underdevelopment;
- a certain role in the occurrence of this complication may play the age of primipara (younger than 18 years old or older than 30 years);
- excessive neuropsychic tension (anxiety, fear of the upcoming birth, negative emotions).
According to the classification existing in obstetrics, there is a distinction between primary and secondary weakness of labor, which can develop in both the first and second stages of labor. With primary weakness of labor, contractions from the onset of labor are weak and ineffective, while with secondary labor and duration of contractions are initially sufficient, but later during labor, contractions gradually weaken, become less frequent and shorter, and no further dilatation of the cervix occurs. Secondary weakness develops less frequently than primary, and, as a rule, is the result of prolonged and painful contractions that lead to fatigue of the parturient.
Diagnosis of poor labor
The diagnosis "weakness of labor activity" is made by the obstetrician, the leading childbirth, based on the nature of contractions, the dynamics of cervical dilatation. The presence of this pathology is indicated by a decrease in the rate of disclosure of uterine throat. So, if it is normal, from the beginning of a regular labor to the opening of the uterine mouth, it lasts 3–4 cm on average for 6 hours, then with the development of the weakness of the labor, this period lengthens to 8 hours or more. During childbirth, the doctor examines the woman in labor at regular intervals. If for a certain period cervical dilatation is not enough, then they also speak of a weakness of labor activity. The doctor-obstetrician works out the tactics of further management of labor after the diagnosis of each particular woman in labor.
Treatment of weak labor
The main non-drug method, which allows to strengthen the generic activity, is amniotomy (autopsy of the fetal bladder). This manipulation is carried out with the disclosure of the cervix by 2 cm or more. Further within 2 3 hours the woman in labor is observed. In some patients, as a result of amniotomy, an increase in labor activity occurs. For example, in case of polyhydramnios, the uterus muscles are over-stretched, and the outpouring of amniotic fluid contributes to a decrease in the intrauterine volume and the onset of proper and sufficient contraction of the uterus muscles. If the desired effect from amniotomy is not obtained, then the use of drugs is necessary. It should be noted that with prolonged childbirth, fatigue of the woman in labor, medical sleep-rest can be used to treat the weakness of labor, during which the woman restores strength and energy resources of the uterus. After awakening in some patients, labor activity increases. In order to conduct a medical sleep-rest, a woman from the group of narcotic analgesics is injected intravenously after consulting an anesthesiologist; sleep comes quickly enough and lasts an average of 2 hours.
It is necessary to emphasize that the main method of treating the weakness of the labor forces is the use of uterotonics - drugs that enhance the contractile activity of the uterus. Oxytocin and prostaglandins have a uterotonic effect. These drugs are administered intravenously, and in modern clinics they use special devices - infusomats, which provide strictly metered administration of drugs. At the same time, the condition of the fetus is monitored with a heart monitor. This therapy leads to an increase in labor activity and often increases pain sensations at the parturient woman. In this regard, there is an additional need for the use of antispasmodics, analgesics, or epidural anesthesia. The duration of the administration of drugs that enhance uterine contractions is determined by the obstetrician, depending on the dynamics of cervical dilatation, the advancement of the part and the condition of the fetus.
Oxytocin does not adversely affect a healthy fetus. However, in case of chronic suffering of the fetus, which often occur in the presence of any complications of pregnancy (gestosis, prolonged threat of termination of pregnancy, placental insufficiency, etc.), administration of Oxytocin may worsen the condition of the fetus. Therefore, before the beginning of birth stimulation, his condition is carefully evaluated according to the nature of the amniotic fluid (in case of chronic intrauterine hypoxia the fetus may have a green color) and according to the results of cardiomonitoring observation.
It should be noted that delays in childbirth in case of development of weakness in labor causes serious consequences on the part of the mother and fetus, therefore, if there are indications in time, the stimulation performed will be the key to a successful outcome of labor.
Unfortunately, the use of the therapy described above is not always effective, and in 18–20% of births with persistent weakness of labor, labor ends with a cesarean section. With the secondary weakness of labor activity, which developed at the end of the expulsion period and is not amenable to medical treatment, it is sometimes necessary to apply a vacuum extractor (fetal extraction using a special apparatus, the cup of which sticks to the head due to air dilution), or (much less often) obstetric forceps one .
Prevention of poor labor
Preventive measures to prevent the weakness of labor include: physio-psycho-prophylactic training (with a set of special exercises and physical exercises), taking vitamins from 36 weeks gestation, which increase the energy potential of the uterus (B 6, folic, ascorbic acid), rational nutrition, compliance regime of the day, as well as the creation of conditions of psychological comfort for a pregnant woman.
In conclusion, it should be noted that the timely diagnosis and correct treatment of the weakness of labor in most cases allows for births through the birth canal and to ensure the birth of a healthy child.
1 Obstetric forceps - a tool used to extract the fetus by the head, if necessary, to immediately complete childbirth.
Elena Karaganova
Doctor obstetrician gynecologist TsPSiR,
Assistant of the Department of Obstetrics and Gynecology of the Russian State Medical University, Ph.D.
Discussion
Again, this article came across .... Add a little. First, the birth of Karaganova in the PMC now cost about 8 thousand dollars 8-0 Secondly, the stimulator of labor activity Dinoproston (and analogues) are forbidden to use, because cause birth bleeding, up to the death of the woman in labor (emergency in the 17th hospital, which led to a change in leadership was associated with this drug). The question remains open - what the hell was I giving it at absolutely quiet physiological labor with good disclosure?
Informative. It is a pity that my cervix did not read this article and does not know that it is supposed to open at a speed of 3-4 cm in 6 hours. And weak, ineffective fights go on for many hours, and then suddenly become strong and effective. And why are babies who are prescribed to suffer from the weakness of labor activity, give birth to 9/10 points, and the older one, who was expelled by “harmless” oxytocin, was born with a 6/7 rating and still has neurological problems?
When our doctors will learn not to customize the birth to the standard? A rhetorical question ...
Drug sleep - anchoring action. I was injected without such consent - I didn’t have enough sleep or rested, and I was even more tired! And the birth itself lasted 16 hours! Without sleep, I think, they would have managed it faster ... Only all sorts of rubbish was poured into the body ...
So the second time I would never agree to this dream.
All familiar faces:) I, Elena Yaroslavovna Karaganova, gave birth to the eldest daughter in 2001. For the "treatment" of the "weakness of labor activity" in the opening of 5 cm. She gave a tablet of Dinoprostone, saying that it was Spazmalgon. (actually stimulated, accelerated childbirth, although I strongly urged all interventions to coordinate with me). Neither in honey. map, nor in the exchange, this drug did not appear later. Cardiac monitor child did not put. Although it happened in the "Samom" TsPSiRe. For reference: Dinoprostone is a hormonal drug (based on progesterone), which has a number of side effects (from the reference book: From the urinary system: hypertension myometrium, tetanic contractions. From the digestive system: nausea, vomiting, diarrhea. Effect on the fetus: fetal arrhythmias , fetal compression, asphyxia. Others: headache, dizziness, hot flashes, tremors, hyperthermia, leukocytosis).
Comment on the article "Weakness of labor activity"
There is no speech about any home births, but if the scar is good, the generic activity is excellent, then why not? But now my friend was denied, her child was already taken out of the birth canal, the scar is very low, no one took up the ep, there will be a ps.
Discussion
kmc depends on the doctor and on the state of the body. after my extras KS complications were not. To be honest, I don’t want to repeat the option “I’ll try it myself + the CS if I’ve done it (they did the stimulation, there was no activity, the slow disclosure + the child did not fall). it's better to be cut right away.
i know cases when, after a cesarean (the difference between children of 3 years), at the age of 37, I also gave birth in a natural way at home. I would not have been able, given the age, Caesarean - it is scary to give birth at home. But she liked everything, gave birth as a 25-year-old and without breaks and complications ..
But the generic activity did not affect and without oxytocin cost. Although side effects there were: vomiting (I didn’t read what they write below, I’ve done a lot of stuff. But as far as I understand it, that kind of. activity weakens after anesthesia is norm. Of course, nothing good, but ...
Discussion
I gave birth all three times without her, but I don’t have a choice either - it doesn’t affect me))
I gave birth without an epidural, it seems to me that you can really endure your contractions and give birth to yourself, but giving birth to oxytocin is a tin. I, of course, suffered, but it is incomparably more painful. If I had to, I would ask for anesthesia. In general, the pain threshold is different for everyone. My girlfriend yesterday gave birth to a fourth child, the last three under the epidural. She says that after her first labor, she does not give birth without epidural anesthesia)
What a nice topic! I am now in trouble myself, for: I gave birth to the first in less than 2 hours, I managed to get to the hospital, but there was no change of mind. From the minuses I see only that labor activity happens to be bad from artificial stimulation .... here I am suffering ...
Discussion
i went to the first place in advance because, when I came to the LCD, the doctor looked at me and announced that I had already opened 1cm.
In the maternity hospital, when she was received, she came to the head of the hospital for inspection, she also said "yes, disclosure, well done, that I came ..."
As a result, 11 days I spent there before giving birth!
But then again, I got water right there in the corridor, and exactly 3 hours later I gave birth. In general, there were chances to give birth on the way)))
This time, I thought that I was going to have a current with contractions ... until I found out that there would be twins. With them I would not risk doing it.
I will go to bed in advance.
what's the point? go to bed in advance just like that - it makes no sense. if there is a reason, then it is necessary.
i went to bed with a previous pregnancy in advance, because the whole pregnancy had problems with the placenta - and detachment and hypoxia were questionable and aging was on the verge. so from 39 weeks was supervised
This procedure for the initiation of labor activity is carried out with minimal disclosure of the cervix. I simply wouldn’t have given, it’s better to prepare for the PCB, or just wait until the birth begins and the Girls themselves write below that there’s nothing wrong with that
Discussion
Yulia, I remain with my opinion from your past topic. I personally would choose PKS at 39 weeks in your situation than stimulation at 37.
There were many personal examples and medical advice given below. I do not know what my opinion is based on - I just feel that this is better.
I duplicate my message in your own topic of May 16 (in case you didn’t see it).
In my example:
1st birth - all the doctors decided. Stimulated at 38.5 weeks by Buscopan and "cervix breeding" is what you are offered. Drug. The result - a child weighing 2670 g, but with a strong vaginal tear and episodes.
2nd birth - trusted nature. Spontaneous delivery at 39.5 weeks. A child weighing 3540 g. Without breaks and episodes.
I also have a “general flattened pelvis”, ABOUT less than 90 cm.
It seems to me that the readiness of tissues for childbirth (their elasticity and the ability to stretch and separate, letting the child pass) is much more important than the weight of the child. Therefore, I am in favor of waiting for the natural onset of labor, and not stimulate them at 38 weeks.
Post from 18.05:
"It seems to me that doctors are very wrong when they frighten women of the COP and rush into childbirth.
I also have a narrow basin and two natural childbirth in history :)
Although already at the beginning of the first pregnancy, my mother-gynecologist said - tune in to the COP (I also have myopia -7).
The first time gave birth to a daughter 2670 g, a strong vaginal rupture and episodes.
The second time was expected rather big boy. When, at 38 weeks, my mother measured my stomach and the height of the bottom of the uterus, I counted that the peanut already weighs about 3,400 g (her calculations were later confirmed), and she could not wait to send me to the hospital.
But I had an ironic attitude towards the natural development of events.
I signed a contract with Vidnovsky maternity hospital, where they take vertical childbirth. True, not as vertical as I would like :), but still - you sit in a special transforming chair, slightly leaning back.
5 days before the PDR gave birth to a boy of 3540 g, 56 cm, head 34 cm, with a small tear, without an episode. Contractions lasted 2 hours (arrived with full disclosure, barely had time), attempts - 40 minutes.
So, my conclusions from personal experience and knowledge drawn from books, the Internet and courses:
1) you need to trust your nature. Of course, there are exceptions, but still nature usually gives a woman a child whom she is able to give birth (if she is not disturbed).
2) by the end of pregnancy, the woman's tissues soften, the ligaments become more elastic, the bones of the pelvis diverge (including during childbirth) to skip the child (I felt this very well in the last periods - it was difficult to walk). Therefore, it is important to bring the child to the due date and not to cause premature birth. Let the child be a little more, but the fabrics will be better prepared.
3) It is highly desirable to give birth in vertical postures (not lying) - as in fights, on and on attempts. In a vertical posture with legs spread apart, the pelvic aperture expands, and the force of attraction helps the efforts of my mother's muscles. Childbirth is faster, less likely that childbirth will be delayed. You need to listen to your feelings and take the posture that the body asks. And the gaps are smaller (my experience has confirmed this).
4) Do not rush to attempts, give the tissues time to stretch to avoid tearing. Doctors are often in a hurry (they are afraid for the child, and they just want to do their job as quickly as possible - they may have other mothers as well).
In my attempts, the fights become rare, with long intervals. In the first birth, the doctor, seeing that the contractions had "disappeared," immediately put on an IV with oxytocin. My daughter was born literally in 3 bouts, breaking everything in there. In the second birth, the doctors only sighed, seeing my slow and not very effective attempts. But - they watched the heartbeat (tube, not CTG), when the head appeared - they looked at its color, like a child there, and did not interfere! For which many thanks to them. Since As a result, I did not break, and the episodes were not needed, and the child’s head and everything else was in perfect order.
And more information from the courses on how to prepare fabrics for childbirth so that they are more elastic:
1) perineal massage with oil (I used almond oil) - daily,
2) after 32 weeks. reduce or completely eliminate meat from the diet (it makes the tissues more “tough”), eat light food - cereals, vegetables, fruits, nuts, fish (without being carried away), less flour and sweet.
3) increase consumption of vit. A (carrot juice with cream).
4) increase the consumption of vegetable oil (3-4 tablespoons per day),
5) fish oil - up to 3 g per day - to soften tissues.
6) drink more pure water.
Of course, I did not exactly observe all this, but I tried to move in this direction :)
if everything is ready, then the birth will begin. if the child is not ready, you understand. if you are not ready, then weaker generic is possible in the comments below. In general, successful delivery is a ready neck + good labor activity.
Discussion
In my understanding, stimulation is a necessary measure. When the body itself does not want to give birth at risk to the health of the mother and child. Just so stimulnutsya to give birth when you need - beyond. I lost the water and contractions were not, just because and stimulated. Honestly given 12 hours for independent delivery. But the stimulation did not help - the contractions are going on as in the last period of labor, and the result is almost zero. Rigid cervix failed. If I knew that it was necessary to prepare it in advance, and that I had such a feature, I would have prepared myself. So eks happened.
They write that with the stimulation of pain to give birth. I do not know. I went to bed with the elder in advance (2 days before the date) and I was “prepared”. It was much less painful to give birth than when it came the second time just with contractions (because of a full house there was no possibility to lie down beforehand)
I wore twins very well, but in the end the truth began to be slightly rude to the kidneys, but my son took it and turned his legs down, while he also lay lower, i.e. chances to be born first had great. And a day later I lost the water without labor.
Discussion
i regret that I answer late and I am glad that you nevertheless chose a caesarean. My pride lay perfectly — both upside down, large close to the exit, a little bit deeper ... the doctors said — one would come out, the second would fly out ... as a result ... in the process of leaving the older one, the younger one turned over, put his head in his stomach ... and with each fight folded it in half.
total-emergency caesarean.
thank God, there were enough brains without "giving birth to water" and so on, and under the supervision of a doctor .... it would have ended unknown how ..
Thank you all for your support and advice. My miracle happened. Exactly at 38 weeks, my boys were born by the COP. As much as I didn’t want to give birth myself, but in fact the choice of the doctor was correct. Children for twins were rather big and they were not going to get out. And during the operation, there were still more surprises that no one suspected. Therefore, all that is not done is all for the better. But now I tried everything myself and give birth to the COP. True, I liked the first option more, but you won’t go for the sake of health and well-being of your beloved children.
Generic activity. Medical issues. Pregnancy and childbirth. Ideal childbirth - practical recommendations (part 1). Enema is also a good inducer of labor.
The doctor who leads me to the LCD insists on a planned cesarean, because thinks that my baby was missed in labor, I had a weak labor activity and I also think that it is necessary to choose in advance good doctorso that he watches the last weeks before the birth.
Discussion
I gave birth to a second child myself, although the first Nikitos was also with hypoxia and now has dtsp and epilepsy. Our daughter was very welcome and desired, we also went through a lot of doctors and tests during pregnancy, all doctors terrorized with questions and fears .... found a doctor who understood us and offered to give birth by yourself, because this is the least risky way .. well, etc. more, if you do a cesarean, how will you care for your first special child ?? worried .... childbirth went well and quickly! baby was born strong and healthy! now she is almost 9 months old and she makes us happy every day! and our Nikitos does not lag behind and tries!
Do not be afraid of anything! Everything will be fine!
My neck also did not open in the first birth. True, I was accelerated, they did not wait for contractions. I came with leaking water, they released me smartly and rolled two vials of oxytocin. The contractions went, and the neck is nifiga. After 5 and a half hours, they ran, Prozerin seemed to dig somewhere (I don’t remember the name), they pricked him and voila, the delivery went, because the neck opened. I still think - if I hadn’t been accelerated - if everything was ok or not, maybe, in theory, it was necessary to wait for the fights, well, I think so: ((
And here, during the first birth, at some point my labor activity stopped and I was given a drip with stimulation. Isn't that right? Is it better if the baby in the stomach without water lay?
Discussion
Why no water?
Vodichka all the time new is being developed.
In my case, both the first and second kinds began with the discharge of water.
A few hours later in the hospital at the ultrasound it was clear that there was still a lot of water left :) And the doctors said that EVERYTHING will not spill out.
About stimulation ...
In the first birth after the stimulation, the clan activity stopped. I remember as a nightmare: (and she was exhausted and the child had a bruise on the floor of the head :(
But I can not say that the doctor was wrong. Who knows how it would all end without stimulation?
At the second time, when opening it was almost complete, and every minute I was also stimulated to decide, and under the guise of saline: (At first, in one fight the child advanced so much that I thought I would die: (I tried to run away from the table :) Then the contractions stopped. I gave birth, and then waited 40 minutes. And no stimulation helped until the child was attached to the breast.
I would still not interfere without a special need in the natural process ...
Doctors have instructions - the bout should go so much, the potent period — so much. And it does not depend on the weight with which the child is born - 2.5. kg or 4.5., don't be jealous of the mother's body, one bone is longer adjusted to the size of the baby, the other is faster. And this is all individually. One child can give birth in 3 hours, and another in two days. Doctors are uncomfortable. Therefore, they lie down in advance and prepare for a certain day. Only you came and went for them, and all the problems remain with you. Apparently the child for some reason needs exactly that time to be born, and no more and no less. The midwife told me the case that one woman had a good period of 6 hours and the disclosure went for almost two days, and the child was born large and completely healthy, well, he needed just that time. Of course in the hospital would be immediately cut, no one would have stood so much time and waited. And yet, the water can not flow out at all, they constantly come in and the child does not suffer when the waters are gone.
The estimated date of birth is over, and you are still pregnant. Since the exact exact date of conception is rarely known to anyone, then if you have not yet given birth on the 41st week, then this is the norm. The child has already grown to 49–52 cm and weighs ~ 3.5 - 3.7 kg. You still have a little time to better prepare for the long-awaited meeting with the baby.
The 41st obstetric week of pregnancy is the eleventh month of pregnancy and the 39th week from conception ().
Fetal development at the 41st week of pregnancy
Your baby is fully ready for birth. All its organs and systems are ready to begin to perform their functions outside the womb. Being in the tummy, the baby is getting stronger, gaining strength and adding weight. He looks like a newborn baby.
Internal development
All the major organs - the heart, kidneys, liver and pancreas properly perform their work. Light crumbs have accumulated the necessary amount of surfactant - a substance that helps the lungs to crack down for the implementation of respiratory functions. The intestine is filled with the first feces, which will be released on the first day after birth.
The development of the central nervous system is suspended, it will continue after the birth of the baby. The vocal cords are strengthened, which will soon be used to attract your attention. The bones of the skull continue to harden, which can cause breaks in the birth canal of the mother during childbirth.
The sheaths of the placenta, separating the fetus from the woman’s body, are weakened and become more permeable, which allows the mother’s blood to mix with the baby’s blood. The baby gets your antibodies designed to protect children's body from the onslaught of infections after childbirth. Thus, the mother passes her immune experience to the child.
External development
At this period, the baby looks much more beautiful than one and a half to two months ago. His body was already cleared of the original protective lubricant, which remained only in the most tender places - in the armpits and groin area. The fluff is gone, and the hairs on the head and the marigolds on the fingers continue to grow. Therefore, the birth of a baby with decent hair and long claws at the forty-first week is not uncommon.
Your baby's body shape has become more rounded, and the ear cartilage is more dense. He gains 30 g of fat per day, and his skin looks smooth and pink. The fetus has already grown, there is not enough space in the stomach, so the baby behaves quieter and makes less movements. But you still need to feel at least ten pushes a day.
If the child does not have enough air, his movements and spasms begin to increase. This can cause bowel cleansing. In this case, meconium enters the amniotic fluid, which is painted in a greenish color, and the baby can swallow them. In such a situation, it may be necessary to connect the child to the breathing apparatus.
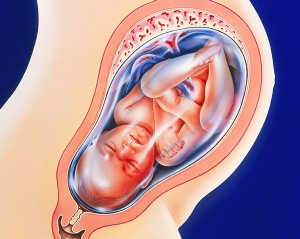
How the fetus is located in the uterus
Normally, the baby at the end of pregnancy is located along the uterus head down. This provides a comfortable passage through the birth canal. If the baby has taken a transverse position or is located head up, then the pregnancy usually ends with a caesarean section. When the fetus does not have a large weight, doctors admit the probability of natural childbirth with breech presentation.
Feelings of a woman at the 41st week
This week for every future mother passes in an anxious waiting for childbirth. Most likely, you are often visited by the same thought: "Already 41 weeks, why the birth does not begin ..." But if you are under the constant supervision of your doctor, do not worry.
Pregnancy is considered postponed when it reaches the 42nd week. Usually the line at 40 weeks is crossed by women carrying the first child.
The cervix continues to be impregnated with hormones, it becomes short and loose, the cervical canal opens. The height of the bottom of the uterus can reach 40 cm, and its elevation above the navel - 20 cm. The amount of amniotic fluid (amniotic fluid) decreases, and the work of your body is aimed at preparing for the upcoming birth process.
Childbirths are coming - forerunners
- Training fights. Most women in the position experience so-called Braxton-Hicks contractions, accompanied by pain as during menstruation. Usually, uterine contractions begin several weeks before delivery, and some begin to bother only a couple of days before them. If contractions are more intense than usual and occur at regular intervals, this means that prenatal contractions have begun, and you need to immediately gather in the maternity hospital!
- Discharge of cork. The mucus plug closing the entrance to the uterus comes out just before the birth or a week or two before they start.
- Omission of the abdomen. The stomach drops a few weeks before the baby is born. The fact that he has already gone down can be understood by reducing the pressure on the stomach and lungs and disappearing.
- Weight loss On the eve of a significant event, your body gets rid of excess fluid, because of which you can observe a slight weight loss.
- Isolation of colostrum. Future mom can detect stains on clothes at chest level. This is a secret secreted from the mammary glands, which feed newborns the first day after birth.
- Frequent urging to the toilet. A growing child is pressing harder on his mother's belly, which makes him constantly run to the toilet.
- Rupture of amniotic fluid. The discharge of water is the same sure sign of the onset of labor as true contractions. Because the appearance on the underwear colorless discharge in any quantity, grab everything you need and go to the hospital.
If you have not seen any signs of a quick birth of a child, it is not scary. Each woman's pregnancy is individual, and many precursors can appear right before the onset of labor.
Pains
It is difficult for a woman in a position to endure the forty-first week, since during this period she can be disturbed by various painful sensations:
- due to the position of the fetus pulls the stomach and lower abdominal pain, with its omission the pain increases;
- the future mother is increasingly concerned about the training bouts, why periodically “turn to stone” stomach;
- the child is pressing on the lower body, which causes pain in the perineum, as well as in the legs and lower back;
- the baby does not move very often, but his movements and blows to the stomach and liver can cause quite a lot of pain;
- itching of the skin of the abdomen;
- numbness of the limbs;
- pinching of the femoral nerve, resulting in painful sensations in the sacrum;
- exacerbation of chronic diseases and their characteristic pains.
At this time, the woman feels clumsy and unwieldy. She is awkward to sleep in almost any position, which can cause restless sleep. Frequent occurrence of the term 41 - swelling of the extremities. The state of health of the pregnant woman is worsened and the irritability attacks arising, seemingly from scratch.
Discharge at week 41
At forty first obstetric week normal light discharges without any strong odor are considered. The appearance of mucus with brown or red veins is also normal. This mucus plug, which can move away at a time, can be allocated in parts.
Before the very birth, you may have amniotic fluid, which looks like a clear, thin, odorless liquid. Often, the water flows in the form of a gushing stream. There are cases when the amniotic fluid is only leaking. If you notice a liquid discharge of green color, this may signal infection of the fetus or that meconium has entered the amniotic fluid. The latter indicates hypoxia. In any case, the discharge of water, you need to urgently gather in the hospital.
The bright red blood found on the panties indicates a threat to the life of your child. In order to avoid placental abruption, consult a doctor immediately!
What to do if childbirth does not start
When the pregnancy has already crossed the threshold at 40 weeks, and the baby still does not want to be born, the mother is afraid to “bear” the baby. But doctors do not consider a 41 week pregnancy postponed. The PDR exposed by the doctor is only the estimated date of delivery, which is calculated by the date of the last menstruation.
But the exact date of birth depends not only on the monthly, but also on a number of other factors, such as the release date and time of fertilization of the egg, the age of the expectant mother and the number of pregnancies transferred by the woman. Therefore, the norm is the birth from the 38th to the 42nd obstetric week. If there are no contractions and there are no signs of childbirth, your doctor may consider prescribing stimulation or cesarean section.
In the absence of contraindications stimulation methods can be applied in the case when:
- as a result of the examination of the condition of the fetus and the bloodstream of the placenta, obvious signs of replanting were detected, that is, the placenta is no longer able to provide adequate nutrition to the fetus;
- if the waters have already withdrawn, and the generic activity does not begin;
- there is a high water flow;
- multiple pregnancy, and the uterus is already strongly stretched.
Medical methods of stimulation of labor include the introduction into the female body of medicines (for example, prostaglandins, mephypristone), the opening of the amniotic sac and mechanical methods. But you can recommend and self-stimulation, which includes the following ways:
- Intimacy with her husband, whose sperm contains prostaglandins, softening the cervix. If the mucus plug is already gone, it is better not to engage in sex.
- Stimulation of the nipples, leading to the release of oxytocin, which increases the tone of the uterus.
- The use of herbal preparations to empty the intestines, provoking an increase in the tone of the uterus.
Apply any methods of labor induction is possible only after consultation with the doctor. He will explain to you how to cause childbirth and how to give birth quickly in your situation.
If the pregnancy proceeds normally, and there is no need for labor induction, you can continue to wait for the meeting with your baby. At this stage, the doctor will be even more closely monitor your health. At the reception in the antenatal clinic, your urinalysis, blood pressure, body weight and abdominal size indicators will be evaluated. It may be necessary to conduct a daily cardiotocography (CTG) procedure that controls the fetal heart activity.
Often, at the 41st week, ultrasound is prescribed. This study allows you to monitor the condition and size of the crumbs, the size of its head, the amount of amniotic fluid, the effectiveness of blood flow to the placenta and the readiness of the cervix for childbirth. If you agreed to hospitalization, all the necessary examinations will be carried out in the hospital.
What is important on the 41st week
- checking the availability of documents and bags for a trip to the hospital;
- medical supervision;
- proper nutrition;
- limiting the amount of fluid consumed and the food eaten;
- day regimen and regular rest;
- moisturizing the skin of the abdomen, chest and thighs or vegetable oil;
- moderate physical activity;
- walks in the open air;
- the development of special breathing techniques, which will be used during childbirth;
- general cleaning of the house together;
- distribution of household duties during your absence;
- communication with baby, still in the tummy;
- doing your favorite thing, which causes you positive emotions.
The 41st week of pregnancy is a great time for mom and dad, who can finish all the necessary things before the birth of a new family member - a daughter or son. Think of this week as extra time that the baby wants to spend in the closest intimacy with you - in your tummy.
Video: stimulation + fees to the hospital
How to understand that the birth began. How to identify contractions
Bag to the hospital
St. Petersburg

Childbirth begins with contractions. At first tolerable, with an interval of 10-15 minutes, then more often, stronger. By the lengthy period, the frequency of contractions reaches 1-2 minutes, and the strength is usually palpable.
Unfortunately, there are cases in which contractions do not increase in strength and frequency, but weaken or are irregular. There may be the fact that training contractions (then you still do not give birth), and maybe - a weak labor activity. What it is, the causes of this anomaly, as well as what a woman can do for her part, and let's talk.
What is it about?
Weak generic activity is of two types.
Primary weakness of labor
The main signs are weak and short contractions, smoothing and opening of the uterus are reduced or terminated. Over time, the duration and frequency of contractions do not increase at all or only slightly.
Depending on the testimony of the health of the woman and the fetus, the doctors conduct the following activities:
- amniotomy (discharge of water enhances contractions);
- drug sleep, for a woman to rest, after the introduction of narcotic analgesics and stimulation with uterotonics (oxytocin and prostaglandins). It usually lasts a dream for two hours;
- the use of drugs that increase the intensity of contractions;
- antispasmodics;
- prevention of fetal hypoxia.
Secondary weakness of labor
It is less common than the primary. Contractions weaken, reduced duration. In this case, the previous phases of labor activity could proceed at a normal pace. Uterus opening and fetal movement along the birth canal slows down or even stops.

As indicated in the book on obstetrics (Obstetrics. National leadership - Aylamazyan EK, Kulakov VI, and others - 2009 - 1200), the main behavior of doctors in the secondary weak labor activity is the introduction of prostaglandins. In the absence or insufficient effect of medical stimulation of labor, as well as the identification of fetal hypoxia, the tactics of childbirth changes. Other methods of delivery are chosen, these can be: cesarean section, use of obstetric obstetric forceps (at this moment I am ready to faint), dissection of the perineum (perineotomy).
Weakness of labor activity is observed in 8-10% of all pregnant women. Moreover, in the first birth the probability is much higher than in the second. This pathology threatens to decelerate the process, exhaustion of the parturient woman (forces on attempts become less and less), fetal hypoxia, infection of the birth canal and inflammatory complications, bleeding during childbirth and the postpartum period. Doctors are forced to conduct drug stimulation labor, which leads to greater pain of the process, as the body does not have time to prepare and develop natural painkillers.
The reasons
For a start, it is worthwhile to understand why there is such a violation of the birth process, and then how to avoid it.
- nervous tension of the pregnant woman, stress;
- genital infantilism (uterine hypoplasia), stiff sweat stiffness (reduced elasticity);
- impaired endocrine and metabolic mechanisms in a woman's body (thyroid gland insufficiency, obesity, diabetes mellitus);
- damage to the uterus (as a result of caesarean section in past births, treatment of endometriosis, uterine myoma);
- overstretching of the uterus (multiple pregnancy, large fruit, high water);
- anatomically narrow pelvis in the parturient woman;
- age of the pregnant woman (up to 18 years old or over 30);
- oligohydramnios and sluggish, flat fetal bladder (as it prevents the child from lowering);
In addition to the above, with secondary weakness of labor, the causes can be:
- maternity fatigue;
- the discrepancy between the size of the baby’s head and the pelvis of the woman;
- malposition;
- the presence in the pelvis of the tumor.
What to do?
With regard to issues of health and physiology, being already pregnant, it is difficult to somehow prepare yourself. Here to help competent doctor, whom you trust. We will consider only what we can influence. And we can influence at different stages, both when preparing for childbirth, and directly in the process.
Preparation before delivery
Vitamins and trace elements
After 36 weeks of pregnancy, doctors prescribe vitamins B6 (pyridoxine), B9 (folic acid), C (ascorbic acid) to prevent it.

For me personally, it was news when I learned that in fact there are products containing a considerable amount of these microelements. And you can get the necessary vitamins, without interfering with the body's work with chemicals. Therefore, I offer you a list of products containing the maximum amount of these three vitamins:
- B6 (pyrodoxin) can be found in walnuts (0.80 mg / 100g), beef liver (0.70 mg / 100g), hazelnuts (0.70 mg / 100g), tomato paste (0.63 mg / 100g), garlic (0.60 mg / 100g);
- B9 (folic acid) is found in large quantities in green asparagus (262mkg / 100g), peanuts (240mkg / 100g), beef liver and chicken (240mkg / 100g), lentils (117mkg / 100g), parsley (117mkg / 100g);
- C (ascorbic acid) can be found in dry rosehip (1200 mg / 100g), fresh rosehip (470 mg / 100g), red sweet pepper (250 mg / 100g), sea buckthorn and black currant (200 mg / 100g), sweet green pepper and parsley (150 mg / 100g). By the way, from time immemorial the recommended oranges and lemons of vitamin C contain only 60 and 40 mg / 100 g, respectively!
To make a decision about replacing vitamins with food, I recommend that you study the issue in more detail and discuss it with your trusted doctor.
Get plenty of rest!
In the last stages of pregnancy, do not forget to rest and sleep well (otherwise, suddenly, tomorrow is war (read, give birth), and the heroic horse (read, pregnant) did not get enough sleep!
Solving psychological issues
With the psychological component of the fear of childbirth can work even during pregnancy. Read more about this.
I happened to talk with a midwife from the city of Berdsk (Novosibirsk region), she told me that the villagers give birth easier than the urban ones. It was positioned from the point of view that residents of large cities are very afraid of pain. Through the prism of my experience, I suspect that the fact is that the village girls are not looking for so much information about childbirth. Do not read the experience of giving birth to other women. “Everybody gives birth. This is a normal process. And I will give birth. "
Pro exercise
I want to warn you about something important. Everything physical exercise during pregnancy should be soft and familiar. That is, you do not need to begin to engage in those types of physical activity that you have never done before.
Surely you heard about the need to perform Kegel exercises to prepare for childbirth? In fact, these exercises are designed to restore the control of urination in women (what’s the point of preparing for childbirth at all ???). Two types of exercises are suggested for pregnant women. In the first one, there is “straining”; in fact, the woman pushes the fetus, which rests on the pelvic floor, because there is no place to push it.
How do you think, are such extrusions useful for the baby? In the second exercise, spontaneous arrest and continued urination are proposed. A similar exercise is done in the classroom on intimate gymnastics, and only under the supervision of a specialist, otherwise you can be tested for incontinence.

Intimate gymnastics is generally a very useful thing, you only need to start it before pregnancy or after childbirth (not earlier than in three, and better in 7 months). Do not create additional stress to the pregnant body, and so it is something to work.
Do you have a lot of questions about caring for a newborn? This is good, because the correct understanding of these topics will serve a good health and
well-being of your child. Pay attention to the excellent courses of doctor Irina Zhgareva, which will help you to orient at the beginning
your motherhood:
"Preparation for pregnancy and childbirth"
“Natural Parenthood: Myths and Reefs”
"Secrets of happy motherhood"
Shortly before the delivery room
Michel Oden, a famous obstetrician-gynecologist, speaks well in his interviews and books about the effects of stress on the process of childbirth. The fact is that during stress, adrenaline is released, which prevents muscle relaxation. The body prepares for protection, fight and stops the generic process. The hormone oxytocin is blocked. All this can lead to weak labor. Therefore it would be good:
Choose the right time
If you plan to give birth in an ordinary hospital, then it is important to go there in time. The contractions are divided into latent (hidden, the uterus is revealed to 4 cm) and active phase. So, in the period of the latent phase, when the contractions are weak enough, you continue to go about your business at home; drink tea, take a shower, etc. As soon as the interval between contractions is 5 minutes. Everything. It's time to maternity hospital. There is at least a war, even a flood, the birth process will not stop. By the way, this option helps to exclude trips to the maternity hospital during training bouts.

Reservation. If your mom had a fast-moving birth, from the discharge — you were allowed to give birth in two hours, then you should be prepared for the fact that you may receive the same bonus inherited. This happens very rarely. But it happens.
Create a comfortable environment.
If possible, create the most favorable environment during childbirth: dim light, no enema, no crowded people (few people will be helped by a large number of people around when contractions), solitude, silence, warmth. It would be nice to shift the task of filling out papers to an assistant. These points are usually discussed with the doctor at the conclusion of the contract.
Use relaxation techniques
During contractions, a warm bath or shower relieves well. However, taking a bath can weaken the process, so a shower is more versatile. Flowing water helps to relax, and this is the main assistant in childbirth.
If you are in the delivery room, and contractions are still weak
The mood of the woman in labor is one of the most important factors. But if something went wrong, you can try the following methods:
- It is necessary to calm down, ask the doctor or the attendant in labor to give a massage, help to take a comfortable posture;
- If you can, do not lie - better to walk;
- If you have to lie down (they make ktg, they put on a drip), then you can lie on that side where the baby’s back is (ask your doctor what side). The back of the baby puts pressure on the uterus, which causes its reduction;
- Emptying the bladder, it helps strengthen the contractions.
I wish you not to be afraid to give birth. Yes, this is an exciting and difficult process, not scary. One experienced mother told me during pregnancy, "it does not hurt to give birth, it is difficult to give birth." And there is one more important momentthat childbirth is not the end of the path; it is the beginning of a new path. You will meet with your baby, it's great! Love your child, this is the most important thing.